An ECG, or electrocardiogram, is a common, painless, noninvasive electrical test administered to record and analyze the electrical activity of the heart.
First performed well over 100 years ago, an ECG can be used to quickly record and diagnose a variety of cardiac conditions.
You may have heard an ECG referred to as an EKG, and in fact the terms are often used interchangeably. They are the same; the K in EKG comes from the German term for the procedure, “elektrokardiographie,” since the procedure was developed by a German-speaking Dutch physician, Willem Einthoven.1
While all ECGs are administered to observe the heart’s electrical activity, there are a variety of lead systems used to record said activity. These have developed over the decades since the procedure was first conducted. For instance, common procedures involve 3, 4, 5, 6, and even 12 ECG leads.
Number and Orientation of Leads
The first lead system for electrocardiography was a three-lead system, also called the Einthoven Lead System, which was developed in 1903.
The Einthoven (3-lead ECG) system traditionally required the patient to submerge his or her right and left arms and left leg in a salt solution. Today, adhesive electrodes are used.2
The number of leads, and placement of electrodes during an ECG, will influence the capture of electrical impulses within the heart that are presented on the ECG graph paper as waves.
The placement of ECG cables and leadwires varies according to the number of leads used in the procedure. Today, one common procedure is the 5-lead ECG. Here’s a primer on what you need to know about what it can show.
5-Lead ECG
Like other ECG lead systems, the 5-lead system uses adhesive electrodes that connect to leads (cables) that capture the signal of the heart and relay it to the box or monitor.
The 5-lead ECG follows the 3-lead configuration with the addition of two more electrodes. One electrode should be placed right underneath each clavicle (black under the left clavicle, white under the right clavicle), with a third at the patient's lower left abdomen just at the lower edge of the ribcage (red). The fourth electrode should be placed adjacent to the sternum on the right side of the fourth intercostal space (brown), and the fifth and final electrode should be placed on the lower left side of the patient’s abdomen (green), at the lower edge of the ribcage. (ECG lead wires are typically color coded, as indicated above.)3
While the 5-lead ECG system provides less detailed information about the electrical activity within the heart, it is less expensive and less difficult to administer than a 12-lead ECG. For routine monitoring, the 5-lead ECG is more than adequate.4
It captures the electrical impulse from the sinoatrial node (SA node) to the atrioventricular node (AV node), then from the Bundle of His and His Branches and finally the Purkinje Fibers which run up the sides of the ventricles.
Many of the cardiac conditions and arrhythmias that a 12-lead ECG can be used to identify can also be discerned from a 5-lead ECG. Among the most common of these are as follows.
- Sinus tachycardia
Sinus tachycardia is a common cardiac arrhythmia in which all of the common waves are present, but are occurring at a rate that is too fast - typically over 100 BPM; in some instances, the heart rate may be so fast that it is difficult to read the P, QRS, and T waves.4
Sinus tachycardia can be caused by a number of common factors, including dehydration, caffeine, stress, fever, and low blood pressure. It can also be caused by underlying medical conditions such as hyperthyroidism.
Fortunately, sinus tachycardia may be the normal result of excessive activity or pain, and is not necessarily cause for immediate alarm. It is, however, important to monitor the patient for additional signs of cardiac distress, such as chest pain or shortness of breath.
- Sinus bradycardia
Sinus bradycardia describes an arrhythmia that is effectively the opposite of ST, which is abnormally slow sinus rhythm. Sinus bradycardia, like ST, manifests all of the P, QRS, and T waves, but at a rate that is slower than normal, or below 60 BPM in a healthy adult.
Sinus bradycardia may manifest without any observable symptoms and in some individuals might be considered normal. For instance, athletes, whose hearts beat more efficiently, sometimes present SB.
In others, SB is typically caused by vagal stimulation and when symptoms are present, such as dizziness, weakness, confusion, or shortness of breath, the situation may become serious.4
Otherwise, in asymptomatic patients, the condition may simply warrant observation until intervention becomes necessary.
- Atrial fibrillation (A-fib)
Atrial fibrillation occurs when signals in the heart’s atria are irregular or chaotic, causing it to flutter instead of beating efficiently. A-fib can manifest as an erasure of the P wave. Instead of a clear P wave, the ECG recording or monitor will show irregular scribbles.4
Controlled atrial fibrillation occurs when the heartbeat is less than 100 BPM and the patient is not experiencing symptoms. Patients can live with controlled a-fib for many years, typically taking an anticoagulant to prevent dangerous blood clots in the atria.4
However, uncontrolled a-fib can become a clinically urgent situation, particularly if the patient feels as though he or she is dizzy or is going to pass out.
In either situation, a-fib is an arrhythmia the goal of which is correction, even if the patient is asymptomatic.
In addition, a 5-lead ECG can also be used to take a biosignal recording of the heart to check for other arrhythmias, for coronary artery disease, to see if the patient has previously suffered a myocardial infarction, or simply to test to see whether or not treatment or implants like artificial pacemakers are working properly.4
Quality ECG Cables and Leadwires
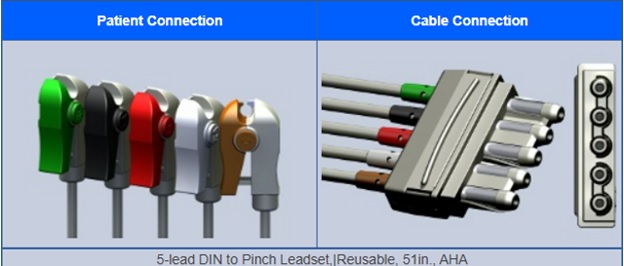
Along with proper patient preparation and electrode placement, a successful, accurate, low-background noise level ECG starts with the use of quality ECG cables and leadwires.
Here at Lifesync, we carry a wide range of ECG cables and leadwires, including 3, 5, and 6-lead ECG cables, EKG cables, radiolucent ECG leadwires, and reusable leadwires. For more information on our collection of quality cables and lead wires, visit the previous link or get in touch with us at 1-800-358-2468 or contact us

